Ganesh_umcvc-aha-research.jpg
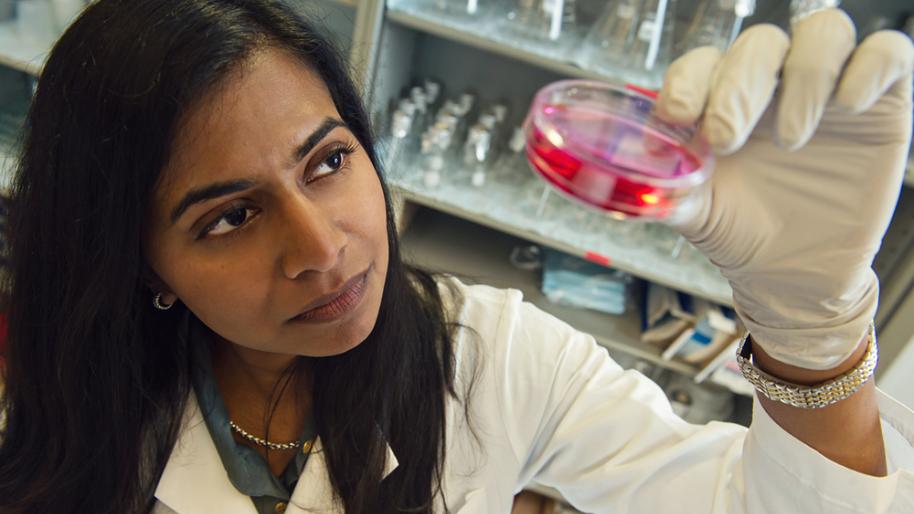
Santhi Ganesh, MD, above, won the 2014 AHA Young Investigator Award
American Heart Walk Fundraising Dollars at Work
The American Heart Association is currently funding over $6.6 million to 42 active research studies at the University of Michigan. As one of the leading academic heart and vascular centers in the world, Frankel Cardiovascular Center researchers can assist the American Heart Association (AHA) in making strides in improving patient care, advocating for better health, reaching out to populations at risk, raising awareness, and protecting the future when it comes to cardiovascular health.
Through fundraising efforts like the annual Washtenaw County Heart Walk, we continue to help fund important research studies like those you see below. Here we shine the spotlight on the AHA-funded researchers and their awards and projects.
Over 12 Years of AHA-Funded Diabetes and Cardiovascular Disease Treatment and Research
Y. Eugene Chen, M.D., Ph.D.
Frederick Huetwell Professor of Cardiovascular Medicine
Professor of Cardiac Surgery, Physiology, and Pharmacology
Vice-Chair for Basic and Translational Research, Department of Cardiac Surgery
Director, Center for Advanced Models for Translational Sciences and Therapeutics University of Michigan
Funded Project: Over 12 Years of AHA-Funded Diabetes and Cardiovascular Disease Research
AHA Award: $2,149,121 (since 2006)

The AHA mission of "building healthier lives free of cardiovascular diseases and stroke" resonates with the ultimate objectives of my research program as a whole and my personal drive as a cardiovascular and metabolism investigator. The AHA 2020 Impact Goal—to improve the cardiovascular health of all Americans by 20 percent while reducing deaths from cardiovascular diseases and stroke by 20 percent—is personally shared by myself and my research team at Michigan Medicine. Our shared vision of reducing the burden of Cardiovascular Disease is the driver to continue contributing not only as an investigator but also as a recipient of the American Heart Association Merit Award and a volunteer.
My scientific career has been successfully developed with the strong support from AHA in the past 20 years. I was the recipient of the AHA Postdoctoral Fellowship (1998-2000), Beginning-Grant-in-Aid (2000-2002), and Established Investigator Award (2008-2012). Also, I have a demonstrated commitment to the mission of the AHA and to advancing the ideals and guiding principles through volunteer service.
Developing New Treatments for Inherited Cardiomyopathies
Sharlene Day, M.D.
Associate Professor, Department of Internal Medicine, Department of Molecular and Integrative Physiology
Funded Project: Disruption of Proteostasis in Hypertrophic Cardiomyopathy Caused by Truncating Mutations in Myosin Binding Protein C
AHA Award: $140,000 (1/2017-12/2018)

Dr. Day and her team are actively involved in institutional and multi-center research studies that aim to learn more about inherited cardiomyopathies and to develop new treatments to prevent the onset of symptoms or reduce their severity. A major focus of her clinical research is determining the importance of fitness for patients with hypertrophic cardiomyopathy (HCM) and establishing evidence-based guidelines to inform recommendations for athletes with cardiomyopathies.
The primary goal of this project funded by the AHA, is to help us understand the basic disease mechanisms in HCM caused by mutations in a specific protein. She hopes that her findings will lead to new areas of investigation in the field and to enable the development of new therapies that target the disease process itself. Her results may also be applicable more broadly to other genetic cardiovascular diseases that afflict millions of families worldwide.
Frankel Cardiovascular Center Summer Undergraduate Research Fellowship Program
Daniel Michele, Ph.D.
Professor, Department of Molecular and Integrative Physiology, Department of Internal Medicine
Funded Project: Samuel and Jean Frankel Cardiovascular Center Summer Undergraduate Research Fellowship Program
AHA Award: $60,000 (2/2017-1/2020)

While the goal of my research laboratory is to study the mechanisms of genetic cardiomyopathies, the funding we received from the American Heart Association supports our Frankel Cardiovascular Center Summer Undergraduate Research Fellowship (SURF) program. This program provides undergraduate students interested in science, medicine, and research the opportunity to experience working in a laboratory focused on cardiovascular disease.
We hope that this program encourages the brightest young minds of the future, but to to pursue a career in cardiovascular research. From our program, to eventually the workplace, we hope these students will use the knowledge they learned in the SURF program to discover new treatments for cardiovascular diseases that continue to be the major cause of death in the United States and the world.
AngioAid – A Fully Automated Computer-Based Platform for Interpreting Coronary Angiograms
Kayvan Najarian, PhD
Associate Professor of Computational Medicine and Bioinformatics
Associate Professor of Emergency Medicine
Funded Project: AngioAid – A Fully Automated Computer-Based Platform for Interpreting Coronary Angiograms
AHA Award: $90,910 (4/1/2017-3/31/2019)

The goal of this research, funded by a grant from American Heart Association (AHA), is to exploit recent advancements in signal processing and machine learning algorithms to construct a fully automated, computer-based platform — AngioAid — that efficiently assists cardiologists with coronary angiogram video evaluation. Preliminary work by our group suggests such a platform is feasible. The AHAs Innovative Development Grant will provide support to further develop this new digital health technology and assess its use more broadly. Ultimately, AngioAid and related innovative tools will disrupt the flawed paradigm of using visual estimation to interpret coronary angiograms.
The research intends to create an assistive system –AngioAid– that would provide clinicians and caregivers with a more reliable and quantitative assessment of coronary angiogram, and as such, it can help improve the quality of the care provided to patients. Additionally, it is expected that the use of AngioAid would reduce the overall cost and therefore the financial burden on both patients and healthcare systems.
