Knee Replacement Surgery
Surgery Overview
Joint replacement involves surgery to replace the ends of bones in a damaged joint. This surgery creates new joint surfaces.
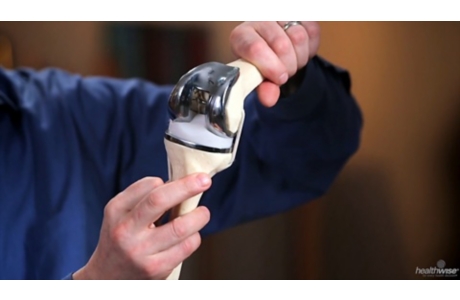
In total knee replacement surgery, the ends of the damaged thigh and lower leg (shin) bones and usually the kneecap are capped with artificial surfaces. These surfaces are lined with metal and plastic. Doctors usually secure parts of the knee joint components to the bones with cement.
Doctors are working on ways to replace just the damaged parts of the knee joint. This is sometimes called partial joint replacement. Unicompartmental replacement is one example of partial knee replacement. It replaces just the inner knee surfaces or the outer knee surfaces, depending on where the damage is. Another partial replacement is called a patellofemoral replacement. In this surgery, the end of the thigh bone is replaced. Then an artificial surface is used to line the back of the kneecap.
Your doctor may use regional anesthesia. This means you can't feel the area of the surgery. You'll have medicine that makes you unaware and lightly asleep. Or your doctor may use general anesthesia. This means you'll be asleep during surgery. Which type of anesthesia you get depends on your doctor and on your overall health. Your doctor might also ask what you prefer.
If you need any major dental work, your doctor may recommend that you have it done before the surgery. Infections can spread from other parts of the body, such as the mouth, to the artificial joint and cause a serious problem. But some experts don't agree that this is likely to happen.
How It Is Done
Normal knee joint
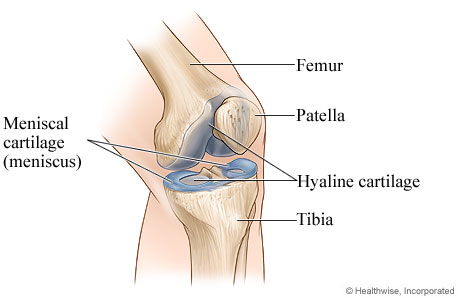
Inside a normal knee joint, thick cushioning (cartilage) covers and protects the ends of your bones. This is called hyaline cartilage. Another type of cartilage, called meniscal cartilage or meniscus, acts like a shock absorber between the bones and keeps the knee joint stable by spreading out the load evenly across the joint. The two menisci (plural of meniscus) protect and cushion the surface of the joint and the ends of your bones.
Osteoarthritis of the knee
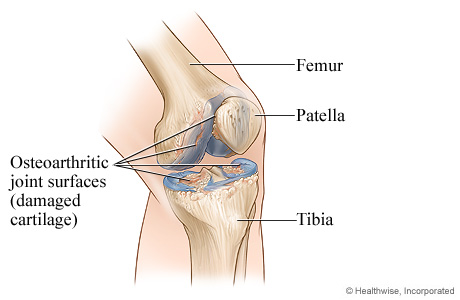
In osteoarthritis, the cartilage that protects and cushions the knee joint breaks down over time. As the cartilage wears down, the bone surfaces rub against each other. This damages the tissue and bone, causing pain. Osteoarthritis is common in the knee joints.
Femoral component is placed
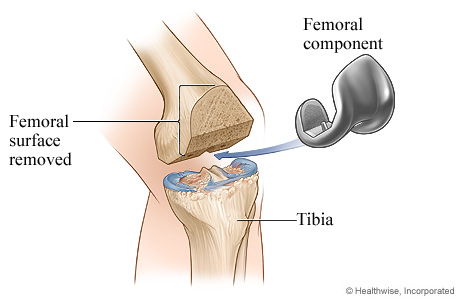
Removal of damaged cartilage and bone from the lower end of the femur and placement of the femoral component
Tibial component is placed
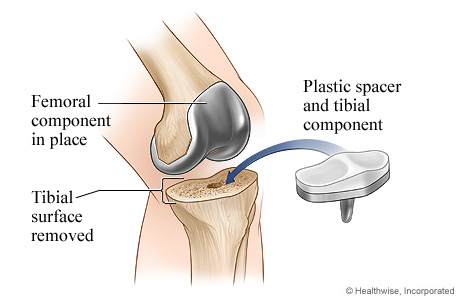
Removal of damaged cartilage and bone from the upper end of the tibia and placement of the tibial component
Patellar component is placed
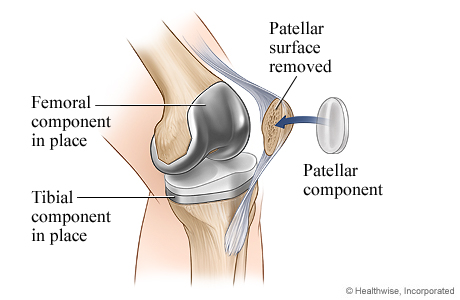
Removal of damaged cartilage and bone from the patella and placement of the patellar component
Knee replacement surgery is complete
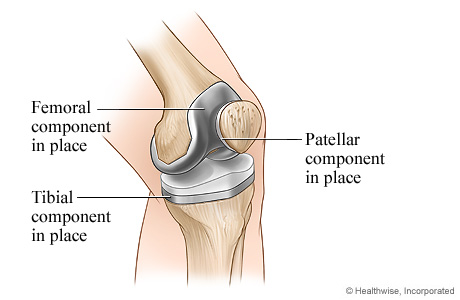
Completed knee replacement
What To Expect
In the hospital
After knee replacement surgery, you will be taken to the recovery room. In a few hours, you may go to a hospital room. You may see a metal triangle called a trapeze over your bed. You can use this to help move yourself around in bed. You will be very tired and will want to rest. Your nurse may also help turn you as you rest.
You will be getting fluids into your vein through an I.V. tube. You may also have a tube called a drain near the cut (incision) in your knee.
You may not feel hungry. You may feel sick to your stomach or constipated for a couple of days. This is common. Your nurse may give you stool softeners or laxatives to help with constipation.
You may have stockings that put pressure on your legs to prevent blood clots. Your nurse will also give you medicine and exercise instructions to help prevent clots.
Most people get out of bed with help on the day of surgery. Your doctor will let you know if you will stay in the hospital or if you can go home the day of surgery.
Your recovery
An artificial knee will allow you to do normal daily activities with less or no pain. You may be able to hike, dance, or ride a bike. Talk to your doctor about whether you can do more strenuous activities.
You'll start rehabilitation (rehab) right after your surgery, usually on the same day. Rehab will help you strengthen the muscles of the knee and regain movement in your knee.
Your doctor will let you know if you will stay in the hospital or if you can go home the day of surgery. When you go home, you will be able to move around with crutches or a walker. You may need some extra support or help at home for the next few weeks until your energy level returns and you can get around more easily.
Your knee will be swollen and will hurt when you move it. You will need to take pain medicine for a time after surgery. Most people will start to walk with a walker or crutches the day of surgery. You will also start to do simple leg exercises. You will probably need about 4 to 16 weeks before you can get back to your job. Your knee may be sore for up to 3 months.
The rehab after a knee replacement takes a lot of time and effort. You will have to stretch and do exercises daily to strengthen your knee and regain movement. The goal of rehab is to bend the knee at a 90-degree angle, which is like the letter "L." But most people who complete all of the physical therapy do better than that.
Living with a knee replacement
You need to stay active after you finish rehab to keep your new knee flexible and strong. You should be able to walk, swim, dance, and ride a bike on flat ground. But you may not be able to run, and you should ask your doctor about riding a bike up steep hills.
Your doctor may want to see you from time to time for several months or more to monitor your knee replacement. Over time, you will be able to do most of the things you could do before surgery.
In the future, make sure to let all health professionals know about your artificial knee so they will know how to care for you.
Learn more
Watch
Why It Is Done
Doctors recommend joint replacement surgery when:
- X-rays show bones and cartilage are damaged.
- Knee pain and loss of function are severe.
- Medicine and other treatments no longer help with pain.
Doctors may not recommend knee replacement for people who:
- Have poor general health and may not tolerate anesthesia and surgery well.
- Have an active infection or are at risk for infection.
- Have osteoporosis (significant thinning of the bones).
- Have severe weakness of the quadriceps muscles at the front of the thigh.
- Have a knee that appears to bend backward when the knee is fully extended (genu recurvatum), if this condition is due to muscle weakness or paralysis.
- Are severely overweight. Replacement joints may be more likely to fail in people who are very overweight.
- Have very high expectations for how much they will be able to do after surgery. These include doing sports that stress the knee.
Some doctors will recommend other types of surgery if possible for younger people and especially for those who do strenuous work. A younger or more active person is more likely than an older or less active person to have an artificial knee joint wear out.
Learn more
Watch
How Well It Works
Most people have a lot less pain after knee replacement surgery and are able to do many of their daily activities more easily.
- The knee will not bend as far as it did before you had knee problems. But the surgery will allow you to stand and walk for longer periods without pain.
- After surgery, you may be allowed to resume activities such as riding a bike, swimming, walking for exercise, dancing, or cross-country skiing (if you did these activities before surgery).
- Your doctor may tell you not to run, play tennis, squat, and do other things that put a lot of stress on the joint.
Most knee replacements (about 90 out of 100) last about 20 years.footnote 1
The younger you are when you have the surgery and the more stress you put on the joint, the more likely it is that you will later need a second surgery to replace the first artificial joint. Over time, the components wear down or may loosen and need to be replaced.
Your artificial joint should last longer if you are not overweight and you do not do hard physical work or play sports that stress the joint.
If you wait to have surgery until you have already lost a lot of your strength, flexibility, balance, endurance, and ability to be active, then after surgery you might have a harder time returning to your normal activities.
Risks
Risks from knee replacement surgery include:
- Blood clots.
People may get a blood clot in a leg vein after knee joint replacement surgery. Blood clots can be dangerous if they block blood flow from the leg back to the heart or move to the lungs.
- Infection in the surgical wound or in the joint.
Infection is rare in people who are otherwise healthy. Some people are at higher risk of infection after any surgery. This includes people who have other health problems, such as diabetes, rheumatoid arthritis, or chronic liver disease. Other risk factors include obesity, smoking, and taking corticosteroids.
- Nerve injury.
In rare cases, a nerve may be injured during the surgery. This is more common in knees that have an unusual shape prior to surgery. These injuries usually get better over time. In some cases, they may go away completely.
- Problems with wound healing.
Wound healing problems are more common in people who take corticosteroids or who have diseases that affect the immune system, such as rheumatoid arthritis and diabetes.
- Lack of good range of motion.
Some people are not able to bend their knee far enough to allow them to do their regular daily activities, even after several weeks of recovery. How much you can bend your knee after surgery depends a lot on how much you could bend your knee before surgery. If this happens, the doctor may give you a medicine to relax your muscles and then gently force your knee to bend farther.
- Dislocation of the kneecap (patella).
This is uncommon. If it happens, the kneecap may move to one side of the knee, and it will "pop" back when you bend your knee. This may not be painful, but it may make the knee feel unstable, and it may be uncomfortable. Dislocation of the kneecap interferes with the way your thigh muscles (quadriceps) work. It usually needs to be treated with surgery.
- Fracture of the kneecap (patella).
The kneecap could fracture either because of a fall or while you are using the knee normally. This complication is very uncommon. Doctors usually can treat a fractured kneecap without surgery.
- An unstable joint.
The knee may be unstable or wobbly if the replacement parts aren't properly aligned. You may need a second surgery to align the parts correctly so that your knee is stable.
- The usual risks of anesthesia.
Risks of any surgery are higher in people who've had a recent heart attack and those who have long-term (chronic) lung, liver, kidney, or heart disease. Obesity also increases the risk.
Credits
Current as of: July 17, 2023
Author: Healthwise Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: July 17, 2023
Author: Healthwise Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Healthwise, Incorporated, disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use. Learn how we develop our content.